Palliative Care providers have the difficult task of trying to ease the suffering of terminally ill patients or patients with end-stage diseases. Unfortunately, in such a supportive role, billing for palliative care, whether in a hospital setting or community, is complex and somewhat limiting.
Overall, there are 5 Palliative care fee codes that you can use when aggressive treatment of the underlying disease process is no longer taking place. When this happens, care is then directed to maintaining the comfort of the patient, until death occurs.
Keep in mind the Palliative Care fee codes are only valid if you’re visiting a patient that is terminally ill and suffering from:
- malignant disease or AIDS,
- end-stage respiratory, cardiac, liver and renal disease,
- end-stage dementia with life expectancy of up to 6 months.
***Bookmark this page for easy-referencing, or for a printable PDF that you can hang up in your workspace scroll to the bottom.
General Palliative Care Fee Code Restrictions & Guidelines:
- You can use palliative care fee codes if your patient is in acute care hospitals, hospice facilities or other institutions – they are not restricted to patients who are in a palliative care unit.
- You cannot use palliative care fee codes if your patient unexpectedly dies from a diagnosis that is unrelated to the diagnosis that they were originally hospitalized for.
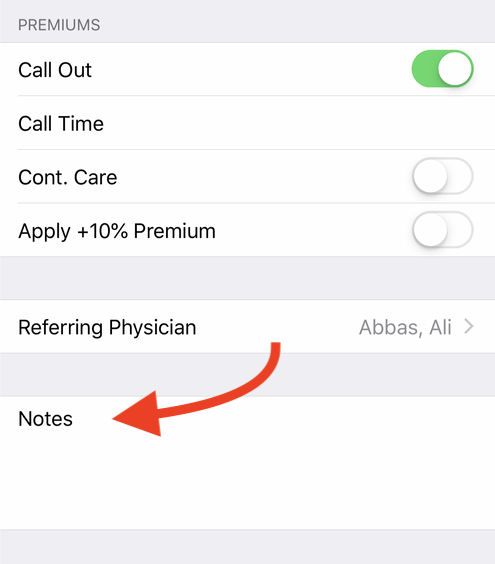
- All palliative care fee codes can be billed continuously once the patient is given a palliative status, for a period not to exceed 180 days prior to death. If you submit palliative care claims that go beyond 180 days, you need to leave a note in the MSP note field explaining why. MSP will then consider your reasons and either approve or reject it.
If you’re looking for more cheat sheets or general instructions on how to master billing, check out our complete guide to MSP billing.
MSP Palliative Care Fee Codes & Guidelines
- 00127 Terminal care facility visit
- 13338 First facility visit of the day bonus
- 13228 Supportive visit
- 13005 Phone call (advice about patient in community care)
- 14063 GP Palliative Care Planning fee
1. Terminal care facility visit: 00127 Palliative Care Fee Code
Bill this with diagnosis V667.
After billing this fee code once, you’ll only be able to bill it for necessary visits for a period not to exceed 180 days (6 month life expectancy).
If your patient’s condition changes for the better and you expect that their life expectancy will now exceed 180 days, you can go back to billing 00114. If you do this, just make sure you leave a note In the MSP note field explaining why. Something like this would do:
- Patient’s condition has changed, life expectancy to exceed 180 days.
Palliative Care Fee Code 00127 Guidelines:
- If you make essential non-emergent additional visits to a hospitalized patient (whether you’re the attending physician or the replacement physician), you can bill them under 00127. The claim must include the time of each visit and a statement of need included in the MSP note field.
- For weekday daytime emergency visit, use fee item 00112.For additional emergency visits (on the same day for the same patient) in the evening, at night or over the weekend, when you’re called back (whether your attending or the replacement) because your patient’s condition has changed or for something that’s unrelated to the hospitalization, bill the following fee codes:12200 Visit – out of office (age 0 – 1).
13200 Visit – out of office (age 2 – 49).
15200 Visit – out of office (age 50 – 59).
16200 Visit – out of office (age 60 – 69).
17200 Visit – out of office (age 70 – 79).
18200 Visit – out of office (age 80 plus) . - For additional visits, when you’re on-site, use one of the following:00113 On call, on site hospital visit (Evening).
00105 On call, on site hospital visit (Night).
00123On call, on site hospital visit (Saturday, Sunday or Holidays). - Your claim must include the time of service and an explanation for the visit included in the MSP note field.
- Chemotherapy fee codes (33581, 33582, 33583, 00578, 00579, and 00580) may not be billed when palliative care patient facility visit fees are being billed.
2. First Facility Visit of the day Bonus: 13338 Palliative Care Fee Code
This is billable in addition to the 00127 for your first patient of the day.
Palliative Care Fee Code 13338 Guidelines:
- Paid only if 13008, 13028, 00127 are billed on the same day.
- You can only use 13338 once a day, regardless of the number of facilities you need to attend.
- Not payable on the same day if you’ve already billed 13339.
3. Supportive Visit: 13228 Palliative Care Fee Code
This is the fee code for supportive visits if you are not the primary palliative care doctor. You need to leave a note in the MSP note field briefly explaining what you did in order to justify the reason/show it’s necessity.
Palliative Care Fee Code 13228 Guidelines:
- Payable once per calendar week per patient, up to the first four weeks. Thereafter, payable once per two weeks up to a maximum of 90 days. For visits over 90 days please you need to submit a MSP note record.
- Payable only for patients in acute, sub-acute care or palliative care.
- Not payable with any other visit fee code including: 00108, 13008, 00109, 13109, 00114, 00115, 00113, 00105, 00123, 00127, 12200, 13200, 15200, 16200, 17200, 18200, 12201, 13201, 15201, 16201, 17201, 18201, 00128, 13028, 13015, 12220, 13220, 15220, 16220, 17220, 18220, 00121, 00122, 12210, 13210, 15210, 16210, 17210, 18210, 00116, 00112, 00111.
- If your on-site and called for emergent care, the following fee codes are billable:00113 On call, on site hospital visit (Evening).
00105 On call, on site hospital visit (Night).
00123On call, on site hospital visit (Saturday, Sunday or Holidays). - A written record of the visit must appear in either the patient’s hospital or office chart.
- If your a hospitalist or a GP member of an Unassigned In-Patient Care Network, and you’re providing GP care to the patient, you may bill 13228. This also applies to Community based GPs with active hospital privileges at a hospital other than the one to which the patient is admitted.
4. Phone call (advice about patient in community care): 13005 Palliative Care Fee Code
This fee may be claimed for advice by telephone, fax or in written form about a patient in community care in response to an enquiry initiated by an allied health care worker specifically assigned to the care of the patient.
Community Care comprises of residential, intermediate and extended care and includes patients receiving home nursing care, home support or palliative care at home.
Allied health care workers are defined as: home care coordinators, nurses, (registered, licensed practical, public health, and psychiatric), psychologists, mental health workers, physiotherapists, occupational therapists, respiratory therapists, social workers, ambulance paramedics, and pharmacists (including completion of faxed medication review with orders, up to twice per calendar year, but not for simple prescription renewal).
Palliative Care Fee Code 13005 Guidelines:
- Claims should be submitted under the personal health number of the patient and should indicate the time of day the request for advice was received.
- When submitting 13005 make sure the dates of services are documented in the patient’s record together with the name and position of the enquiring allied health care worker and a brief notation of the advice given. Alternatively, the original fax, or a copy of written advice, will suffice to document these services.
- You cannot claim this fee code in addition to visits or other services provided on the same day for the same patient.
- This fee may be billed to a maximum of one per patient, per physician, per day.
- You cannot claim this fee code for advice in response to enquiries from a patient or their family.
- You cannot claim this fee code if your employed or are under contract to a facility in which your duties would otherwise include this type of care. Similarly the fee code does not cover advice provided by doctors who are on-site, on-duty in an emergency department, who are being paid at the time on a sessional basis, or who are working at the time as hospitalists.
5. GP Palliative Care Planning fee: 14063 Palliative Care Fee Code
This is billed for the development and documentation for a care plan for your patient. This means that in your clinical judgement your patient has reached the palliative stage of a life-limiting disease or illness, and they now have a life expectancy of up to 6 months. The patient needs to consent to the focus of care now being palliative.
Remember that Palliative Care fee codes are available only if your patient suffers from:
- malignant disease or AIDS,
- end-stage respiratory, cardiac, liver and renal disease,
- end-stage dementia with life expectancy of up to 6 months.
Patient Eligibility:
- Eligible patients must be living at home or in assisted living. Patients in Acute and Long Term Care Facilities are not eligible.
- Requires documentation of the patient’s medical diagnosis, determination that the patient has become palliative, and the patient’s agreement to no longer seek treatment aimed at a cure.
- The patient must be eligible for BC Palliative Care Benefits Program (even if they haven’t applied for the palliative care benefits program, just as long as they are eligible).
Palliative Care Fee Code 14063 Guidelines:
- This fee requires a face-to-face visit and assessment of the patient. If the patient is incapable of participating in the assessment to confirm and agree to their being palliative, then the patient’s alternate substitute decision-maker, or legal health representative, must be consulted and asked to provide informed consent.
-
Payable once per patient, once the patient is deemed palliative. Under circumstances when the patient moves communities after the initial palliative care planning fee has been billed, it may be billed by the new GP who is assuming the ongoing palliative care for the patient.
- Payable in addition to a visit fee (home or office) on the same day if medically required and does not take place concurrently with the face-to-face planning included under 14063.
- You must spend a minimum of 30 minutes on the care plan. 16 minutes of this must be face-to-face with your patient or their medical representative.The non-face-to-face planning (review chart and existing care plans, medication reconciliation, etc.) may be on different dates and may be delegated to College-certified allied care provider (e.g., nurse, nurse Practitioner), working within the eligible physician practice. Chart documentation must include:1. the care plan;
2. total planning time (minimum 30 minutes); and
3. face-to-face planning time (minimum 16 minutes).
- 14063 is only payable if you’re a family physician who commits to providing the majority of your patient’s longitudinal comprehensive care. The Care Plan requires documentation of the following in the patient’s chart:
- There has been a detailed review of the case/chart and of current therapies.
- Name and contact information of the substitute decision-maker.
- Documentation of eligible condition(s).
- There has been a face-to-face planning visit with the patient, or the patient’s medical representative if appropriate, on the same calendar day that Care Planning Incentive code is billed.
- Specifies a clinical plan for the patient’s care.
- Documentation of the patient’s current health status including the use of validated assessment tools when available and appropriate to the condition(s) covered by the care planning incentive.
- Incorporates the patient’s values, beliefs and personal health goals in the creation of the care plan.
- Outlines expected outcomes as a result of this plan, including advance care planning when clinically appropriate.
- Outlines linkages with other allied care providers who would be involved in the patient’s care, and their expected roles.
- Identifies an appropriate time frame for a re-evaluation of the plan.
- Provides confirmation that the care plan has been created jointly and shared with the patient and/or the patient’s medical representative and has been communicated verbally, or in writing, to other involved allied care providers as appropriate. The patient and/or their representative/family should leave the planning process knowing there is a plan for their care and what that plan is.
- 14077 is payable on same day, for same patient, if all criteria are met. (Time spent on conferencing does not apply to time requirement for 14063).
- Not payable if 14033 or 14075 has been paid within 6 months.
- Not payable on same day as 14043 , 14076 or 14078.
- 14050, 14051, 14052, 14053, 14033, 14066, 14075 not payable once Palliative Care Planning fee is billed and paid because the patient has been changed from active management of chronic disease and/or complex condition(s) to palliative management.
- The GPSC Mental Health Initiative Fees (14043, 14044, 14045, 14046, 14047, 14048), are still payable once 14063 has been billed, provided all requirements are met. However, they are not payable on the same day.
- Not payable to physicians who are employed by or who are under contract to a facility and whose duties would otherwise include provision of this care.
- Not payable to physicians working under salary, service contract or sessional arrangements whose duties would otherwise include provision of this care.
Palliative Care MSP Billing Tips
If you’re interested in other MSP fee codes, save a link to our MSP searchable database below. You can search by specialty, billing code or keyword.
MSP billing codes Searchable Database
Explanatory Codes
If you submit a claim and it doesn’t pass the approval process by MSP your claims may be rejected, reduced or refused. This can happen for a variety of different reasons (around 706 different reasons to be exact)!
In our experience, these are the most common scenarios to watch out for:
- Location of fee code doesn’t match. Ie, radiologic fee code performed in ER
- There’s a fee code conflict – so assessment is required
- Invalid use of Premiums
- No Referring Physician
- Patient doesn’t have insurance
Extra Reminder: A lot of errors are a direct result of either not adding a referring physician OR not double checking that your patient has insurance. So, make sure you always check these two things before submitting a claim.
When it does occur, you’ll be given an explanatory code for why each rejection, reduction or refusal happened. To find out what the code means find a description below:
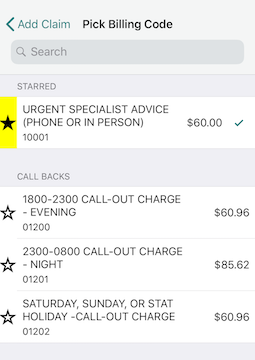
Starring:
If you’re billing with Dr.Bill you have the option of ” starring” your most commonly used billing codes. That way, they’ll appear at the top for easy-searching.
If you found this useful, or would like to see more MSP billing tips, let us know on twitter.
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.







