If you’re an internal medicine specialist in Ontario knowing which fee code to use can quickly get confusing. The complexity of submitting claims to OHIP, on top of your already heavy workload, is bound to cause a few headaches.
To help save you time, we’ve put together an internal medicine guide of all the available fee codes and when/how to use them. Knowing which codes are available in your speciality is essential in order to maximize your earning potential.
Internal Medicine OHIP Billing Guideline for Consultations & Assessments
In general most internal medicine consultations are allowed once per 12-month period. All types of consultations (as outlined below) need to have been referred to you by a physician or nurse practitioner.
A repeat consultation is only allowed once per 12-month period if pertaining to the same diagnosis. A second consultation is only payable in a 12-month period if the diagnosis is completely different than the first. A limited consultation is allowed 1 per 12-month period.
What’s the difference between consultation and a limited consultation? Typically a limited consultation would take up much less of your time and wouldn’t require as much, if any, of taking a medical history.
General Assessments are allowed once per 12-month period. A general assessment requires less time spent with the patient than a consultation. Generally, a consultation is requested by another physician where as an assessment could be an appointment the patient booked, or that you saw in an emergency setting.
If you need to see your patient again (for the same diagnosis) you can use a general reassessment – you can bill 2 of these per a 12-month period. You can also bill partial assessments which are unlimited.
What’s the difference between a general assessment and a partial assessment? A General Assessment would include full history where as the partial assessment is limited in that you don’t need to take their history. A general assessment is typical when you see a patient for the first time and don’t know their history.
Outpatient Internal Medicine OHIP Billing Codes
For outpatients, set the service location code to HOP and the facility number of the hospital to AM. A is the prefix for outpatient.
A135 Consultation
A765 Consultation patient 16 years and under.
A130 Comprehensive Consultation – minimum time spent 75 mins. Stop and start times recorded in patient record.
A435 Limited Consultation
A136 Repeat Consultation
A133 Medical Specific Assessment
A134 Medical Specific Re-Assessment
A120 Colonoscopy Assessment – same day as colonoscopy.
K045 Diabetes Management by a Specialist.
- Maximum of 1 service per patient per 12 month period, eligible if you’ve previously provided a minimum of 4 of the following – consultations, assessments, K013, K033, K029, K002, K003 in the 12 month period.
K046 Diabetes Team Management
- Maximum of 1 service per patient per 12 month period, eligible if you’ve previously provided a minimum of 4 of the following – consultations, assessments, K013, K033, K029, K002, K003 in the 12 month period.
Visit to Emergence Department for Consultation or Assessment
*Use the A prefix and add a premium for time and travel if you were outside the hospital when called.
Emergency Department: Special Visit Premium
| Weekdays | Mon. – Fri. “Sacrifice of Office hours” | Evenings M-F | Weekends & Holidays | Nights | |
|---|---|---|---|---|---|
| Travel Premium | K960 : $36.40 Max. 2 | K961 : $36.40 Max. 2 | K962 : $36.40 Max. 2 | K963 : $36.40 Max. 6 | K964 : $36.40 Unlimited |
| First Person Seen | K990 : $20.00 Max. 1 | K992 : $40.00 Max. 1 | K994 : $60.00 Max. 1 | K998 : $75.00 Max. 1 | K996 : $100.00 Unlimited |
| Additonal Person(s) Seen | K991: $20.00 Max. 9 | K993: $40.00 Max. 9 | K995: $60.00 Max. 9 | K999: $75.00 Max. 19 | K997: $100.00 Unlimited |
In Patient Internal Medicine OHIP Billing Codes
For inpatients, set the service location code to HIP and the facility number of hospital to acute care. C is the prefix for inpatient.
C135 Consultation
C765 Consultation, patient 16 years of age and under
C130 Comprehensive Internal Medicine Consultation – minimum time spent 75 mins. Stop and start times recorded in patient record.
C435 Limited Consultation
C136 Repeat Consultation
C133 Medical Specific Assessment
C134 Medical Specific Re-Assessment
C131 Complex Medical Specific Re-Assessment
E082 MRP Premium – Add this to Admission consultation or admission assessment.
In Patient: Special Visit Premium
When using a special visit premium to travel for inpatients make sure the consult/assessment always uses the prefix A.
| Weekdays | Mon. – Fri. “Sacrifice of Office hours” | Evenings Mon. – Fri. | Weekends & Holidays | Nights | |
|---|---|---|---|---|---|
| Travel Premium | C960 : $36.40 Max. 2 | C961 : $36.40 Max. 2 | C962 : $36.40 Max. 2 | C963 : $36.40 Max. 6 | C964 : $36.40 Unlimited |
| First Person Seen | C990 : $20.00 Max. 1 | C992 : $40.00 Max. 1 | C994 : $60.00 Max. 1 | C986 : $75.00 Max. 1 | C996 : $100.00 Unlimited |
| Additonal Person(s) Seen | C991: $20.00 Max. 9 | C993: $40.00 Max. 9 | C995: $60.00 Max. 9 | C987: $75.00 Max. 19 | U997: $100.00 Unlimited |
Subsequent Visit Internal Medicine OHIP Billing Codes
C132 First 5 weeks per visit.
C137 6th to 13th week, 3 per week.
C139 After week 13, 6 per month.
E083 MRP Premium – Add to subsequent visits when you are MRP.
Subsequent Visit (by MRP) Internal Medicine OHIP Billing Codes
C122 Day 1 following MRP admission – add E083.
C123 Day 2 following MRP admission – add E083.
C124 Day of discharge – add E083, if the patient in hospital for at least 48 hours.
Subsequent Visits by MRP following transfer from Intensive Care Unit
C142 Day 1 after transfer – add E083.
C143 Day 2 after transfer – add E083.
***Note: the patient must be admitted to ICU by a different specialty.
C121 Additional visits due to intercurrent illness.
C138 Concurrent Care.
C982 Palliative Care.
Long Term Care In Patient Internal Medicine OHIP Billing Codes
For inpatients, set the service location code to HIP and the facility number of the Long Term Facility. For long term care make sure your patient card has an admission date. Long Term Care facilities are considered an extension of a hospital, they are “inpatients” therefore an admit date is needed.
W235 Consultation
W765 Consultation patient 16 years of age and under.
W130 Comprehensive Consultation – same as A130.
W435 Limited Consultation
W236 Repeat Consultation
Admission Assessment
W232 Type 1
W234 Type 2
W237 Type 3
W239 Periodic health visit.
W134 General Re-Assessment.
Long Term Care Facility: Special Visit Premium
When using a premium for time and travel for Long Term Patients make sure the consult/assessment is the prefix A.
| Weekdays | Mon. – Fri. “Sacrifice of Office hours” | Evenings Mon. – Fri. | Weekends & Holidays | Nights | |
|---|---|---|---|---|---|
| Travel Premium | W960 : $36.40 Max. 2 | W961 : $36.40 Max. 2 | W962 : $36.40 Max. 2 | W963 : $36.40 Max. 6 | W964 : $36.40 Unlimited |
| First Person Seen | W990 : $20.00 Max. 1 | W992 : $40.00 Max. 1 | W994 : $60.00 Max. 1 | W998 : $75.00 Max. 1 | W996 : $100.00 Unlimited |
| Additonal Person(s) Seen | W991: $20.00 Max. 9 | W993: $40.00 Max. 9 | W995: $60.00 Max. 9 | W999: $75.00 Max. 19 | W997: $100.00 Unlimited |
Subsequent Visits
W132 First 4 visits per patient per month
W131 Additional visit (max 6 per patient per month)
W982 Palliative Care
Nursing Home or Home for the Aged
W133 First 2 visits per patient per month
W138 Subsequent visits per month (max 3 per patient per month)
W972 Palliative Care
W121 Additional visits due to intercurrent illness.
COMMON BILLING SCENARIOS
Scenario 1:
You’re called in to the ER on a Saturday evening at 7p.m. for a consultation. You head to the hospital and see the patient. Your claim would look like this:
A135 (outpatient consult)
K963 (travel premium)
K998 (first person seen premium)
The Service Location Indicator (SLI): HOP
Facility number: the # for Ambulatory Care
After the consultation – If your patient is then admitted, you would also bill the following:
E082 (Admission Assessment by the MRP)
The Service Location Indicator (SLI): HIP
Facility number: the # for Acute Care
If the patient was already an inpatient when you were called into the hospital then you’d bill the following:
C135 for inpatient consult or
A135 for inpatient consult IF claiming Special Visit Premiums. OHIP will only pay Special Visit Premiums on consults and assessments if it’s the A prefix code, even for an inpatient (which is the C prefix code). They will know it is an inpatient by the Special Premium Visits that are used.
Scenario 2:
You’re in the hospital and rounding on inpatients, one of your patients has been admitted for less than 5 weeks. Your claim would look like this:
C132 (subsequent visits).
However – if you’re rounding on inpatients and you’re the MRP you’d bill the following:
C122: day following the hospital admission assessment
C123: second day following the hospital assessment
C124: day of discharge
For subsequent visits with the same patient (as the MRP) you can also add the following premiums)
E083 (adds a 30% premium to the subsequent visit code)
E084 (adds a 45% premium to the subsequent visit code if provided on Saturdays, Sundays and holidays);
Reminder: Special Visit Premiums are NOT eligible with subsequent visits. If the physician was called in to see the patient on an urgent matter, subsequent visits shouldn’t be billed.
Scenario 3:
At the hospital, you see a patient for a consult who is 15 years old. Your claim would look like this:
C130 (comprehensive internal medicine consultation inpatient).
However, if you saw the patient outside of the hospital you’d only need to change the prefix:
A130 (comprehensive internal medicine consultation outpatient)
Common Billing Mistake: Getting rejections on Counselling Codes
We often see rejections of counselling codes due to the following reasons:
- Billing special visit premiums on counselling codes.
- Billing counselling (such as K013) on the same bill as an assessment with the same diagnosis code.
Counselling appointments are technically pre-booked and therefore no special visit premiums apply.
However, counselling codes CAN be billed on the same day as an assessment BUT:
- They need to be on separate claims.
- They need to have different and unrelated diagnostic codes.
*** With the exception of the codes listed below, no other services are eligible for payment when rendered by the same physician on the same day as any type of counselling service.
Exceptions:
E080
WCB Claims
You get paid for both the insured insurances you provide and for reports, there are two different ways to submit claims:
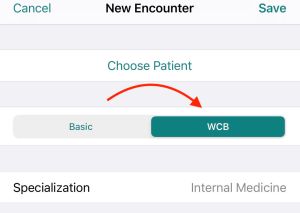
- Insured Services: Submit a claim to OHIP like you normally would except on the claim you’ll indicate “WCB.” OHIP will then pay you for your services and bill WSIB accordingly. If you’re using Dr. Bill, select WCB at the top of the claim instead of OHIP like this:
- WSIB Forms: When you fill out a form, you bill WSIB. You need to upload these claims directly to WSIB through the online portal Telus Health. These claims have different fee codes than OHIP, which outline which form you’re using.
- WSIB Physician Fee Schedule
If you’re interested in other OHIP fee codes, make sure to save a link to our OHIP searchable database below. You can search by specialty, billing code or keyword.
OHIP billing codes Searchable Database
This article offers general information only and is not intended as legal, financial or other professional advice. A professional advisor should be consulted regarding your specific situation. While information presented is believed to be factual and current, its accuracy is not guaranteed and it should not be regarded as a complete analysis of the subjects discussed. All expressions of opinion reflect the judgment of the author(s) as of the date of publication and are subject to change. No endorsement of any third parties or their advice, opinions, information, products or services is expressly given or implied by RBC Ventures Inc. or its affiliates.

Additional Reading
Dr. Nour Khatib left medical school for a finance career, but a persistent calling encouraged her to return years later and become an emergency physician.







