Submitting claims for payment can be complicated, and when billing MSP your claims may be rejected, reduced or refused. This can happen for a variety of different reasons (around 706 different reasons, to be more precise).
When it does occur you will be given an explanatory code for why each rejection, reduction or refusal happened.
Dr.Bill users enjoy a 97% payout success rate — but for those claims that do get rejected, reduced or refused, here is a description of each explanatory code:
Explanatory Codes
- *A — Our records indicate patient deceased. Please contact MSP.
- *B — Patient’s eligibility with MSP is in question. Please have patient contact MSP.
- *C — MSP is unable to locate patient. Please have patient contact MSP.
- *D — MSP has been unable to contact patient. Please have patient contact MSP.
- *E — Our records indicate patient has permanently moved outside of B.C. Please have patient re-apply for coverage if applicable.
- *F — Patient has opted out of MSP. Patient should be billed directly.
- *G — Our records indicate MSP is not the primary insurer for this patient.
- *H — Our records indicate the patient requested coverage to be cancelled.
- *I — Date of service is prior to coverage effective date.
- *L — Lab Volume Discount (excluded)
A
- AA — PHN is missing or invalid.
- AB — PHN is not on our records.
- AC — This is not a valid PHN for MSP.
- AD — This is an incorrect PHN for this patient.
- AE — This claim is the responsibility of the interim Federal Health Program.
- AF — This patient does not have coverage for the DOS.
- AG — This service billed as “A Donor” coverage.
- AH — Dependent number is missing or invalid.
- AI — Dependent is not registered.
- AJ — This is an incorrect dependent number.
- AK — Coverage for this dependent has been cancelled.
- AL — This dependent is not eligible for coverage with MSP.
- AM — Dependent number and/or initial(s) do not match our records.
- AO — First name or initial(s) does not match our records.
- AP — Initials and/or surname are missing or invalid.
- AQ — Surname does not match our records.
- AR — Birthdate missing or invalid.
- AS — Baby not registered.
- AU — A claim for this service has been paid on the mother’s PHN, under dependent # 66.
- AV — Technical difficulties with coverage check. Contact Teleplan support.
- AW — Claim must be submitted with PHN.
- AX — Province contacted, name and health number not matching.
- AY — Provincial/insurer or institution code missing or invalid or fee item not valid for insurer.
- A1 — Patient signature required on pay patient account.
- A2 — Patient address required on pay patient account.
- A5 — Referred to or by doctor number is not valid for DOS.
- A6 — Child is over-age for dependent 66.
- A7 — Dependent 66 – PHN submitted is registered to male. Please resubmit using mother’s PHN and dependent 66.
- A9 — PHN not approved for ICBC claim number.
B
- BA — Initials and/or surname changed to match CareCard. Please confirm correct initials and surname with patient.
- BB — PHN changed to match CareCard.
- BC — Surname/initials and PHN changed to match CareCard.
- BD — Child not registered. Processed under dependent 66.
- BE — PHN changed to newborn’s PHN.
- BF — Claim is held for future processing.
- BG — Amount adjusted to the rate effective for this DOS.
- BH — This claim will be processed on a future remittance statement. Please do not re-bill.
- BI — Fee item and diagnosis do not correspond.
- BJ — Fee item and amount billed do not correspond.
- BK — Your claim submission is being held pending WorkSafeBC notice of approval.
- BL — Massage therapy discounted.
- BN — The maximum number of additional areas has been paid for this date of service.
- BP — Birthdate submitted does not match our records.
- BR — Please clarify the date of service.
- BU — Claim was received prior to date of service.
- BV — Service date exceeds allowable claim submission period.
- BW — Hospital visits must be submitted with each month on a separate line.
- BX — Claim is being held pending ICBC notice of approval.
- BZ — MSP has consolidated two PHNs held by this person. Please update your records to the PHN indicated.
- B2 — Previous PHN has been replaced with PHN indicated. Please update your records.
- B3 — In future, please bill multiple services of the same fee item on one line (eg. 13621 x 3; 09921 x 3)
- B4 — Patient now has B.C. coverage. Please contact patient and re-bill under the correct PHN.
- B5 — Child is over-age for billing under mother’s identity number under the reciprocal agreement.
C
- CA — Fee item and time stated do not correspond.
- CB — Number of services and time stated do not correspond.
- CC — Please state time anesthetic commenced.
- CD — Date of service and fee item billed do not correspond.
- CE — DOS was not a Saturday, Sunday or statutory holiday.
- CF — Time called or time service was rendered is missing or invalid.
- CG — Each service must be on a separate line.
- CH — Please clarify billing; writing is illegible.
- CI — Number of services and amount billed do not correspond.
- CJ — Date of service and amount billed do not correspond.
- CK — Practitioner number is invalid for this payment number and date of service.
- CL — Payment number is invalid for this date of service.
- CM — Specialty is invalid for this date of service.
- CN — Practitioner is not registered with the College of Physicians and Surgeons or not active with MSP for this date of service.
- CP — Practitioner status invalid for date of service and type of submission.
- CQ — Practitioner is not licensed to bill for this service.
- CR — (531) WorkSafeBC incentive applied for proof submission. Please refer to the contract for more information.
- CS — (530) WorkSafeBC penalty applied for invoice submission. Please refer to the contract for more information.
- CT — (532) WorkSafeBC amount adjusted to non-contracted rate.
- CU — We are unable to process this account as this is an invalid referral.
- CV — (534) WorkSafeBC penalty applied for proof of timeliness. Please refer to the contract for more information.
- CW — Telephone advice fees may not be charged when another service was provided on the same day.
- CX — (529) WorkSafeBC incentive applied for invoice submission. Please refer to the contract for more information.
- CY — (527) WorkSafeBC invoice amount was adjusted to contract rate.
- CZ — (562) WorkSafeBC amount adjusted to $0.00 refer to fee schedule or contract.
- C1 — Contract with invalid.
- C2 — Special program name invalid.
- C3 — Assessment diagnostic invalid.
- C4 — Treatment plan prescription missing or invalid – please specify.
- C5 — Primary disposition missing or invalid.
- C6 — (524) WorkSafeBC daily maximum for good/service has already been reached.
- C7 — (525) WorkSafeBC invoiced units reduced to approved units for good/service.
- C8 — (528) WorkSafeBC invoice amount was adjusted to the Fee Schedule.
- C9 — (532) WorkSafeBC penalty applied for proof submission. Please refer to the contract for more information.
D
- DJ — This claim is the responsibility of ICBC.
- DP — Your claim has been debited as our records show that the patient was out of province for the date of service.
- DR — Debit adjustment. See secondary explanatory code(s).
- DS — Account debited to agree with fee item paid to surgeon. Please re-bill for payment.
- DV — Item 00012 is not payable with laboratory blood work or visit fee charges to the same or an associated physician on the same date.
- DW — Debit adjustment of MSP claim as WorkSafeBC hospital emergency per diem rate billed for same date of service.
- DX — ICBC has refused responsibility for your office visit. Insurer responsibility has been adjusted to MSP, therefore 13705 does not apply and has been withdrawn.
- D0 — Match found for debit request record.
- D1 — Debit request record did not meet Pre-Edit or Edit requirements.
- D2 — No match found for debit request record.
- D3 — Payment withdrawn per debit request record.
- D4 — Unable to perform debit request at this time. Claim is currently in process. Please review account with processed.
- D8 — Debit adjustment of account paid at GP rates.
- D9 — Original claim is at WorkSafeBC and your debit request has been forwarded to WorkSafeBC.
E
- EA — Fee items 00101, 12101, 12201, 13201, 15201, 15301, 16101, 16201, 17101, 17201, 18101 or 18201 are not payable to emergency room physicians.
- EB — Standby time is not payable by the Plan.
- EC — Services provided by the Canadian Blood Service are not a benefit of the Plan.
- ED — There is insufficient medical necessity to process this claim.
- EE — This service is not an insured benefit of the Plan.
- EF — Not a benefit under the Reciprocal Agreement.
- EG — This service is the responsibility of WorkSafeBC
- EH — Mileage is not a benefit except for unusual emergencies.
- EI — Service not listed in the Payment Schedule. Please contact your Association.
- EJ — Services at the request of a third party are not an insured benefit of the Plan.
- EM — Service unrelated to MVA injury.
- EP — (512) WorkSafeBC service is not allowed with another service already paid on this date of service. Please refer to the contract.
- ER — (520) WorkSafeBC pre-requisite item not received or rejected. Please check contract for pre-requisite required and your previous billing information.
- ET — (516) WorkSafeBC invoiced units reduced to remaining approved units.
- EX — This claim has been paid as a WorkSafeBC account.
- EZ — These fees are not a benefit when used for overtime compensation.
- E1 — This service appears to be performed during your APP contracted hours – therefore it is not billable to MSP.
- E2 — (521) WorkSafeBC limit 1 form 8 per claim, rate adjusted to Form 11 fee.
F
- FA — Previous claim incorrectly refused/adjusted by the Plan.
- FB — This is a duplicate claim. An identical claim is being processed.
- FC — This account has been paid or refused in accordance with previous correspondence, phone call or note record.
- FE — Payment adjusted per information received.
- FF — Payment for the full fee has been paid to another physician; we do not split the fees.
- FG — Age of patient does not correspond with the fee item billed.
- FH — Service by definition is bilateral or multiple.
- FI — Services rendered to a physician’s own family member are not payable.
- FJ — 00112, 01200-01202 only applies to the first patient treated.
- FK — This account was billed under the wrong PHN or dependent number.
- FL — Professional/technical fee paid to another facility. Total fee not payable.
- FM — Repeat graded exercise tests require an explanation of the medical necessity.
- FN — Previously paid service(s) considered to be included, have been deducted.
- FO — The sex of the patient does not correspond with the fee item/diagnostic code.
- FP — This patient’s care is restricted to another physician. Please refer to the MSP bulletin.
- FQ — Adjustment made because of additional information received.
- FR — See explanatory letter.
- FS — Service is refused or adjusted. Information requested has not been received.
- FT — Additional information was not received.
- FV — This service is included in a previously paid item.
- FW — Re-billing submitted to change insurer responsibility.
- FX — This is a reciprocal claim.
- FY — This claim normally requires manual processing. It has been computer paid and is subject to review at a later date.
- FZ — This claim normally requires manual processing but has been computer adjusted or refused. If you disagree please resubmit with details in the claim comment/note field.
- F1 — Included in WorkSafeBC hospital emergency per diem rate.
- F2 — Time/date does not correspond with related claims.
- F3 — Your re-billing is being processed.
- F4 — Operative/procedural report does not substantiate the fee item billed.
- F5 — Group therapy is not paid for more than one member of a family per session.
- F6 — Please check patient identification. This card has been reported lost or stolen.
- F7 — Payment records show that this patient is seeing multiple general practitioners.
- F8 — An adjustment is in process for the remainder of this claim.
- F9 — Payment/refusal of the original claim cannot be reviewed until receipt of a re-billing plus additional details and/or operative/pathology report, if applicable.
G
- GA — A new consultation is not allowed when a group of physicians routinely working together provide a call for each other. Your claim was refused or reduced.
- GB — A referral had not been received at the time of processing.
- GC — A major consultation is not payable if the patient has been seen within 6 months for the same condition.
- GD — This item is payable once per hospitalization. Otherwise, consultation preamble rules apply. If you disagree with this refusal, please resubmit with a note.
- GE — Claim has been refused or adjusted as the service is included in the dialysis fee.
- GF — As there is no indication of medical necessity for a new consultation, your account has been adjusted to the appropriate visit fee.
- GG — This fee is included in the consultation or visit fee.
- GH — Consultation/visit is included in the fee for the procedure.
- GJ — Our records indicate this is a referred case.
- GK — Referral now received.
- GL — A consultation is not payable to the family physician.
- GM — Specialist discharge care plan for complex patients has already been paid to you or another specialist.
- GN — Specialist discharge care plan for complex patients is only payable on inpatients.
- GN — Specialist advance care planning discussion is not paid while patients are receiving critical or intensive care in the hospital.
- GO — Specialist advance care planning discussion is not paid while patients are receiving critical or intensive care in the hospital.
- *NEW* GP – Services billed on the same day as an LFP service require start and end times.
- GQ — Referral now received. Computer generated code.
- GR — Directive care is payable at 2 visits per week.
- GS — Directive care is payable after surgery unless the patient is seen for a different condition.
- GT — (250) WorkSafeBC refused – Electronic report submission. Incomplete form transmission.
- GU — (608) WorkSafeBC – payee is not authorized for date of service. For more information contact Corporate and Health Care Purchasing.
- GV — (514) WorkSafeBC service is not approved or outside allowable entitlement period.
- GW — (501) WorkSafeBC information missing. Please resubmit with missing information.
- GY — This consultation has been paid although it looks like transfer of care (>3 consults/same specialty in 14 days)
- G1 — (157) WorkSafeBC refused – Electronic report submission included an invalid date format.
- G2 — (201) WorkSafeBC refused – Electronic report submission incomplete. Required information missing, employer’s name.
- G3 — (563) WorkSafeBC GST amount exceeds maximum allowable amount.
- G4 — (209) WorkSafeBC refused – electronic report submission incomplete, required information missing, employee’s address.
- G5 — (227) WorkSafeBC refused electronic report submission incomplete required information missing, estimated time off work.
- G6 — (233) WorkSafeBC refused – electronic report submission incomplete. Required information, work restrictions.
- G7 — (564) WorkSafeBC total amount must be greater than Federal tax amount.
- G8 — (565) WorkSafeBC total amount must be greater than Provincial tax amount.
- G9 — (566) WorkSafeBC PST amount exceeds maximum allowable amount.
H
- HA — This claim has been paid to you.
- HB — This claim has been paid to you. Please note the change in name/PHN.
- HC — This claim has been paid under the indicated fee item.
- HD — This claim has been paid to an associated doctor or alternate payment number.
- HE — A retro adjustment has been applied to this paid claim.
- HF — This account has been paid to the physician providing LOCUM services.
- HG — Your account has been refused or debited as the patient was out of province on this/these dates.
- HH — Payment reversed at the request of WorkSafeBC
- HI — Referral has now been received. Payment will remain at specialist rates.
- HJ — This fee has been paid to another physician or facility.
- HK — Credit Adjustment – See secondary code for explanation.
- HL — This claim has been paid for a different date of service.
- HM — This claim does not meet the over-aged submission requirements.
- HN — The information provided does not correspond with our records on file.
- HO — This claim was paid as an ICBC account.
- HP — Your note comment/correspondence has been considered, however, we are unable to alter our previous decision.
- HQ — Computer generated credit.
- HR — This procedure is normally performed once in a lifetime. Please resubmit with an explanation for the repeat procedure.
- HS — A credit adjustment has been processed for this claim.
- HT — This account has been overpaid in error.
- HU — Previously paid amounts for individually billed services exceed per diem rate.
- HV — A claim for this service has previously been processed.
- HW — (507) WorkSafeBC duplicate service. A service was already paid for this date of service. Please do not re-bill.
- HX — This claim has been paid to you. Computer refusal.
- HY — Balance payment. Amount previously paid for individually billed services deducted from per diem rate.
- HZ — Payment for this account was previously withdrawn per your debit request record. If requesting payment, please resubmit with an explanation in your note record.
- H1 — Daily volume limit exceeded. Payment discounted by 100%
- H5 — Daily volume limit exceeded. Payment adjusted.
- H8 — Daily limit exceeded. Paid at 50%.
- H9 — Daily limit exceeded. Paid at 25%.
I
- IA — B prefixed or asterisk items are included in visit/procedure fee.
- IB — 00012/90000 is not payable when performed with other blood work.
- IC — Multiple injections are paid to a maximum of three per sitting.
- ID — Claims for 00081 must be supported with details of bedside/resuscitative services. Please provide break down on a per 1/2 hour basis.
- IE — The Tariff Committee has not recommended approval for this tray service. Patient may be charged for costs.
- IF — A visit fee is not payable with subsequent injections.
- IG — Fee is not applicable unless the physician is called from another site to render the emergency service. Resubmit with details of where you were called from.
- IH — The consult or visit constituted the first half hour of care.
- II — Misc fees must be supported with details of the service provided.
- IJ — 00083 cannot be billed alone. Your claim has been adjusted to the appropriate visit fee.
- IK — Duration of visit is required for this service.
- IL — 00081 includes any minor procedures performed at the same time.
- IM — This service charge is not applicable for the time/date and/or the item billed.
- IN — 01210 – 01212 are not payable with diagnostic procedures.
- IO — Paid according to the time and/or duration stated.
- IP — 00039 is the only fee payable for any visit associated with methadone maintenance.
- IQ — Refractory period is 30 minutes for non-operative continuing care surcharges unless for CCFPP care.
- IR — Minor tray fee not applicable.
- IS — Major tray fee not applicable.
- IT — Tray fee not applicable with fee item billed/paid.
- IU — Tray fee not applicable when service performed in a Ministry funded facility.
- IV — Tray fee not payable to hospitals or extended care facilities, etc.
- IW — The Tariff Committee has recommended approval for the addition of this tray service.
- IX — The Tariff Committee has not recommended approval for the addition of this tray service. Included in overhead.
- IY — Tray fee to be billed by physician performing procedure.
- IZ — Mini tray fee not applicable.
- I0 — ICBC has refused responsibility for this claim; therefore, MSP has accepted responsibility. The insurer code has been changed.
- I1 — Please resubmit with details of the emergency call-out.
- I2 — 01210 – 01212 are not billable with non-emergency procedures.
- I3 — 01200 – 01202 an d01205 – 01207 and 01215 – 01217 only apply when the physician is specially called to render emergency or non-elective services.
- I4 — Please resubmit the remainder of this claim under the applicable fee for continuing care, according to the time indicated.
- I5 — Emergency visits/surcharges are not paid for routine call backs. Please resubmit with details of the medical necessity for additional emergency services.
- I6 — Claims for 00082 must be supported by details of the care provided to critically ill patient. Please provide breakdown on a per 1/2 hour basis.
- I7 — Only one tray fee is applicable when multiple procedures are performed.
- I8 — Our records indicate that another physician is responsible for care under the methadone maintenance program during the same time period. Re-bill with additional information.
- I9 — ICBC has refused responsibility of this claim.
J
- JA — Multiple diagnostic procedures are paid at 100% or the larger fee and 50% for the lesser.
- JB — If a diagnostic procedure takes place on a subsequent visit within 30 days, only the diagnostic procedure is paid.
- JC — The annual limit has been reached.
- JD — Fee items 00931 – 00936, 00942, 00943 are paid at 100 percent when billed together.
- JE — Payment has been made at the appropriate per diem rate based on date(s) and sequence of associated claims.
- JF — When the patient acuity level changes up or down, the appropriate second day rate applied (01521 01522 or 01523).
- JG — Services for pain control/acute pain control are included in Critical Care fees for ventilatory support and/or comprehensive care.
- JH — This service is included in the payment for critical care.
- JI — There is insufficient medical necessity to process this claim. Resubmit explaining the need for services outside the critical care team, if applicable.
- JJ — Written support for medical necessity is required to pay critical care fees within the post-op period. Resubmit with additional information if applicable.
- JK — Information provided does not meet the criteria for the critical care fee item billed. Please resubmit with additional information, if applicable.
- JL — Subsequent non-inclusive surgical procedures rendered by a member of the critical care team are paid at 75%.
- JM — The fee for the first day of critical care has already been paid to you or another physician.
- JN — Critical Care schedule fee items are not payable within the duration of a general anesthetic.
- JO — To be considered for payment claims for fee items 00081/00082 in lieu of critical care fees must be accompanied by a written explanation of medical necessity.
- JP — Critical Care ventilatory support (01412 – 01442) has been paid to another physician. Your claim has been paid/refused according to the Section Preamble.
- JQ — Day 2 rates for Critical Care apply when patient is re-admitted for the same condition.
- JR — Critical care (01411 – 01441) has been paid to another physician. Your claim has been paid/refused according to the Section Preamble.
- JS — Day 2 rates for critical care apply when the service is preceded by a consultation.
- JT — Claims for percutaneous transluminal coronary angioplasty/additional vessel (00840 – 00842) are payable at 75% when billed by a team member.
- JU — Comprehensive care (01413 – 01443) has been paid to another physician. Therefore, we are unable to process your claim for payment.
- JV — When a patient is admitted to NICU after 48 hours, second day rates will apply again (01521, 01522, 01523).
- JW — 01200 – 01202 and 01205 – 01207 and 01215 – 01217 are not payable in addition to adult and pediatric critical care fees (01411 – 01441, 01412 – 01442 and 01413 – 01443).
- JX — When a patient is readmitted to NICU within 48 hours, billing continues at the same rate as if there were no break, unless there is a change in acuity level.
- JY — When a patient is readmitted to ICU within 48 hours with the same or similar problem, billing continues at the same rate as if there were break.
- JZ — When a patient is readmitted to ICU after 48 hours with the same or similar problem, day 2 rates apply.
- J0 — (519) WorkSafeBC payee is not authorized to provide goods/services for more information contact corporate and health care purchasing.
- J1 — (283) WorkSafeBC refused – report submission incomplete, required information missing, work location missing.
- J2 — (568) WorkSafeBC HST not applicable for item.
- J3 — (287) WorkSafeBC refused – report submission invalid, specific reference number invalid or missing.
- J4 — WorkSafeBC refused – report submission incomplete, required information missing, clinical information missing.
- J5 — (281) WorkSafeBC refused – report submission incomplete, required information missing, worker’s city and/or work location missing.
- J6 — (279) WorkSafeBC refused – report submission incomplete, required information missing, injury description missing.
- J7 — (277) WorkSafeBC refused – report submission incomplete, required information missing, patient duration missing.
- J8 — (275) WorkSafeBC refused – report submission incomplete, required information missing, disabled from work flag missing.
- J9 — (273) WorkSafeBC refused – report submission incomplete, required information missing, rehab program not indicated.
K
- KA — There is no indication that two separate visits were made. If two visits were performed, please provide times of each visit.
- KB — Visits and minor procedures, same diagnosis – larger fee only is paid. Different diagnosis – lesser fee paid at 50%.
- KC — Repeat complete physicals within 6 months require an explanation of medical necessity.
- KD — This service does not meet the criteria for fee item billed.
- KE — This fee is applicable between 8 am and 6 pm
- KF — Patient’s annual limit for counselling has been reached.
- KG — Counselling for two or more members of a family must indicate that they were seen individually.
- KH — One 00114 is paid every two weeks for care provided in a long-term care institution (eg. nursing home, intermediate care facility) unless supported by an explanation.
- KI — Another physician has been paid for daily hospital care.
- KJ — The total number of services exceeds the number of hospital days.
- KK — This service is not a benefit of the Plan when performed in a hospital.
- KL — Daily care is payable up to 30 days only unless supported by additional information of the medical necessity.
- KM — Supportive care visits are limited to one visit for the first 10 days of hospitalization then one visit per 7 days per MSC Payment Schedule Preamble D.4.7.
- KN — Out-of-hospital care was provided during this time. Please verify hospitalization dates.
- KO — In-hospital care was provided during this time. Please verify the dates.
- KP — Lab, x-ray and/or interpretation fees are not a benefit under the Plan for a registered bed patient.
- KQ — Our records indicate patient is located in a nursing home. Please verify and re-bill with the appropriate fee item.
- KR — Hospital visits are not payable in addition to the routine care of a newborn.
- KS — Hospital visits have been paid during the period you have billed nursing home care. Please verify location of patient.
- KT — Nursing home visits have been paid during the time you have billed hospital care. Please verify location of patient.
- KU — Please resubmit the remainder of this claim, if applicable, under supportive or directive care.
- KV — Emergency Medicine fees and minor procedures – the lesser fee is paid at 50%.
- KW — Fee item billed does not meet the criteria for group counselling. The appropriate visit fee has been paid.
- KX — Fee item billed is only applicable when service is provided in hospital emergency room. The appropriate visit fee has been paid.
- KY — Visit fee includes examination/assessment of multiple diagnoses.
- KZ — Fee item and diagnostic code/note comment do not correspond.
- K0 — 92515/92516 not payable with 92510, 92520-92544 or 92546.
- K1 — Processed according to the Preamble to the Medical Services Commission Payment Schedule.
- K2 — Processed according to the Section Preamble to the Medical Services Commission Payment Schedule.
- K3 — Processed according to the description of the fee item, or the note relating to the fee item, in the Payment Schedule.
- K4 — Please refer to the protocol for this fee item.
- K5 — Your re-billing has been processed. In future, please ensure that the necessary information (eg. “CCFFP”) appears in the first line of your note record.
- K6 — Primary base fee is not applicable. Your account has been paid under the appropriate split base fee.
- K7 — Patient not registered. Payment for third and subsequent services will be reduced to 50% (Primary Care).
- K8 — Patient not registered – payment reduced to 50% (Primary Care).
- K9 — Our records indicate that fee item 00114/00115 is not applicable. Please verify the patient’s location.
L
- LA — Volume discount mechanism applied as per 2007 renewed lab agreement.
- LB — This item is not a benefit of the plan unless performed in an MSC approved facility or as an outpatient service.
- LC — Your claim for fee item 13075 was refused as MSP has not received an associated claim from you or an ICBC visit (Must be for an unrelated condition).
- LD — Nerve blocks/IV procedures are not paid with time units or procedures.
- LE — Continuous care by a second anaesthetist is paid under time fees only.
- LF — Anesthetic Procedural Fee Modifiers are not payable in addition to diagnostic or therapeutic anesthesia fees.
- LG — Your claim for fee item 13070 was refused as the WSBC visit was claimed for the same or a related condition.
- LH — Anesthetic procedural modifies are only applicable to general, regional and monitored anesthesia.
- LI — Your claim for fee item 13075 was refused as the ICBC visit was claimed for the same or a related condition.
- LJ — Intensity/complexity fees are not applicable to the surgical/diagnostic procedure(s) billed.
- LK — Your claim for fee item 13070/13075 was refused as a procedure was billed for the same or a related condition.
- LL — 13052 is not applicable for a pre-operative examination.
- LM — Insufficient medical necessity for two anaesthetists has been received.
- LN — Please provide duration of continuous time spent with the patient during second and/or third stages of labour only.
- LO — Your claim for fee item 13070 was refused as MSP has received a non WSBC visit claim from you.
- LP — Fee items 01151 and 13052 are not applicable when performed in conjunction with other anesthetic services.
- LQ — Visit fees are not payable at the time anesthetic services are rendered.
- LR — This service is included in the annual complex care block fee.
- LS — Age related annual complex care block fee items must be provided on the same date of service as complex care planning fee item 14033.
- LT — This service is not payable on inpatients who reside in a care facility.
- LU — Your claim has been refused due to an inadequate medical record. The MSC Payment Schedule Preamble C.10 describes the requirements of an adequate medical record.
- LV — This service is limited to once per calendar year per patient and has been paid to another practitioner.
- LW — This service is only payable if the patient is seen and a visit billed on the same date. Please resubmit for both services, if applicable.
- LX — Fee item 33583 is for administering single parenteral chemotherapeutic agents and not for the injection if 1 hrh. Please resubmit using fee item 00100 if applicable.
- LY — Claim for Fee Item 32308/32318 has been paid as Fee Item 00308 as care has exceeded the first 10 days of hospitalization.
- L1 — (510) WorkSafeBC practitioner not authorized for date of service. For more information contact corporate and health care.
- L2 — WorkSafeBC refused – duplicate form detected.
- L3 — (517) WorkSafeBC invoiced units reduced to daily maximum for good/service.
- L4 — (533) WorkSafeBC incentive applied for proof timeliness. Please refer to the contract for more information.
- L5 — (539) WorkSafeBC interest applied.
- *NEW* L6 – LFP fees are not payable on reciprocal patients. Please rebill with the appropriate MSC Payment Schedule fee(s)
- *NEW* L7 – LFP interaction fees are limited to one per patient. If two separate interactions were performed, please provide a note record with the times of each visit.
- *NEW* L8 – This service is included in the LFP Payment Model.
- L9 — (509) WorkSafeBC practitioner number is missing or not recognized. Please add or correct the information on the invoice and resubmit.
M
- MA — Multiple exams performed on the same visit, the lesser exams are paid at 50%.
- MB — A repeat refraction within a 6 month period requires medical necessity.
- MC — Items 02010, 02015 and 02012 include certain individual eye exams.
- MD — Exam and a minor procedure billed on the same day, the lesser fee is paid at 50%.
- ME — Eye exams are not paid with office/hospital visits.
- MF — Referring doctor provided is invalid for payment of consultation billed.
- MG — These exams are paid to a maximum of three per day.
- MH — 02012 is not payable within three days of emergency surgery.
- MI — The appropriate fees for removal of foreign bodies from the surface of the eye are 13610, 13611 or 06063
- MJ — A fee item has been established for this service. Please resubmit under the approved code.
- MK — Fee item 13005 is not payable when the patient is a registered bed patient in an acute care hospital.
- ML — Fee item 13005 may only be billed once per day per physician per patient.
- MN — Fee item 13005 is not payable in addition to services provided on the same day/same physician/same patient.
- MO — A total fee has been paid to the same practitioner or payee. Professional and technical fees are included in the total fee so your claim has been refused.
- MP — Fee item 00109 is not applicable when a patient is referred for continuing care by a certified specialist. The appropriate visit fee has been paid.
- MQ — Fee item 00109 is not applicable when a patient is referred for continuing care by a certified specialist. The appropriate visit fee has been paid.
- MR — Fee item 00109 is not applicable when preceded by a complete physical exam within 7 days by the same physician. The appropriate visit fee has been paid.
- MS — Does not meet the criteria for billed services for hospitalized patients.
- MT — Sub-acute care has been paid during the period you have billed for acute/supportive care. Please verify the location of the patient.
- MV — Acute/supportive care has been paid during the period you have billed for sub-acute care. Please verify the location of the patient.
- MW — This OSMV form fee is not payable on the same date of service as another OSMV form fee that you have billed.
- MX — Driver’s licence number is not numeric, is missing or is not located in the first seven spaces of the note or comment field.
- MY — A repeat OSMV form fee is not payable to any practitioner within 3 months.
- MZ — Insurer is invalid for this service.
- M1 — (269) WorkSafeBC refused – report submission incomplete, required info, regular practitioner indicator missing or invalid.
- M2 — (271) WorkSafeBC refused – report submission incomplete, required info, return to full duties indicator missing or invalid.
- M3 — GPSC conference fee items 14015, 14016 or 14017 have been paid to you on the same date of service. Therefore, this GPSC attachment Fee Item is not applicable.
- M4 — GPSC conference fee items 14015, 14016 or 14017 have been paid to a different GP on the same date of service so this GPSC attachment fee is not applicable.
- M5 — GPSC attachment fee items have been paid to you on the same or prior date of service so GPSC fee items 14015, 14016, 14017 and 14033 are not applicable.
- M6 — GPSC attachment fee items have been paid to another GP on the same or prior date of service so GPSC fee items 14015, 14016, 14017 and 14033 are not applicable.
N
- NA — Payable at 50% when billed with delivery fees.
- NB — Fee item 14094 is payable once within 6 weeks following a C-section or vaginal delivery but not to the physician who performed the C-section.
- NC — 04116 is only applicable in the immediate post-partum phase.
- ND — Pre-natal visit fees are not payable within the post-natal period.
- NE — Included in the fee for delivery, caesarean section or post-natal care.
- NF — Please resubmit with an explanatory note record per the direction provided in the note(s) listed under the fee item.
- NG — Additional prenatal visits must be supported by medical necessity.
- NH — Included in fee items 04025, 04050, 04052, 14108 and 14109.
- NI — Only one prenatal complete examination (00101/14090) is payable per physician per pregnancy.
- NJ — Multiple call backs are not normally paid with delivery. Provide details of serious complication(s) requiring additional emergency care.
- NK — Timing for fee item 14199 begins after two hours of continuous care during second stage of labour.
- NL — This claim has been paid to the obstetrician.
- NM — The incentive for full service GP obstetrical bonus is only applicable when fee item 14104, 14108 or 14109 is paid to the same physician/same day.
- NO — Item 14000 is only payable when the physician attends one delivery on the date billed.
- NP — Fee item 14000 is payable for the first delivery the GP attends on the date billed, to a maximum of 25 bonuses per calendar year.
- NQ — The incentive for full service GP obstetrical delivery bonus is payable for the first delivery the GP attends on the date billed.
- NR — The incentive for full service GP obstetrical delivery bonus is payable to a maximum of 25 bonuses per calendar year.
- NS — You have reached or exceeded the practitioner calendar year limit for this service.
- NV — This fee item is only payable to the physician who has provided the majority of the longitudinal general practice care to the patient over the preceding year.
- NW — This fee item is not payable for services provided by physician who are working under a salaried, sessional or service contract arrangement.
- N1 — (546) WorkSafeBC debit request from payee.
- N2 — (544) WorkSafeBC invoices received date and time cannot be in future.
- N3 — (555) WorkSafeBC invoices original amount cannot be negative.
- N4 — (556) WorkSafeBC invoice must be a debit.
- N5 — (557) WorkSafeBC invoice items created date and time cannot be in future.
- N6 — WorkSafeBC invoice items created date and time cannot be on or before received date and time.
- N7 — (559) WorkSafeBC invoice total amount cannot be negative.
- N8 — (560) WorkSafeBC invoice items unit amount cannot be negative.
- N9 — WorkSafeBC refused – call out charges not payable for service(s) billed.
O
- OA — Primary and secondary wound management fees are only applicable with fees from the Orthopaedic Section.
- OB — Consult/visit is included in the paid claim on the same date of service by the same practitioner or payee for OSMV fee item 96226 or 96227.
- OC — Eye exam is included in the paid claim on the same date of service by the same practitioner or payee for OSMV fee item 96226 or 96227.
- OD — Visual field test 02041, 02042, 02043 is included in the paid claim on the same date of service by the same practitioner or payee for fee item 96226, 96228.
- OH — Adjusted to the appropriate fee/amount for an open reduction and/or compound fracture.
- OI — External fixation is not payable with an open reduction fee.
- OJ — Remanipulation is not payable to the same physician within five days of the initial procedure.
- OL — Primary wound care management fees are not stand alone items. Please re-bill with the appropriate fracture fee if applicable.
- OM — 51037/51038 is only paid with applicable orthopaedic section items.
P
- PA — 00622 has been paid for another dependent. This fee includes parental assessment.
- PB — Consultations for two family members or more require individual referrals and must be seen separately.
- PC — Psychotherapy sessions extending beyond one hour per day must be supported by an explanation of need.
- PD — Family therapy is only payable on one member’s PHN.
- PE — Invalid service clarification code for psychiatry fee item.
- PF — Invalid service clarification code for Rural Retention Premium.
- PG — Specialty invalid for Rural Retention Premium.
- PH — PCO Registration submitted for a PHN that is currently registered to an associated primary care organization.
- PI — Adjustment due to PHN registration change.
- PJ — PHN not registered on service date. Claim for a non physician and/or billed fee item does not meet conversion to fee for service criteria.
- PK — Adjustment due to PHC registration change E-debit only, no matching credit created.
- PL — Rural retention is not applicable to the geographic location where the service was provided.
- PO — Beneficiary reimbursement for services.
- PW — Resubmit as extended services code (960xx) or MSP fee code with an explanatory note.
- PZ — Please resubmit with child’s PHN. Consider registering PHN with the primary care organization.
- P0 — Claim for a non-physician and/or billed fee item does not meet conversion to fee for service criteria.
- P1 — Related claims have been paid by ICBC. Please check your records and re-bill using MVA indicator “Y”, if necessary
- P2 — Partial payment from ICBC for one service.
- P3 — Related claims have been paid by WorkSafeBC. Please check your records and re-bill using insurer code “WC”, if necessary.
- P5 — Not approved for service.
- P6 — PHN not registered to primary care organization.
- P7 — Invalid/missing date in note record.
- P8 — PCO invalid registration cancel date/cancel reason code.
- P9 — Registration not eligible for PCO site.
Q
- QA — An Operative Report is required to assess this claim.
- QB — An Operative Report and the medical necessity is required to assess this claim.
- QC — The medical necessity is required to assess this claim.
- QD — Written support for two assistants is required from the surgeon.
- QE — Service is within the pre or post-operative period.
- QF — Pre and/or post-operative services have been deducted from this claim.
- QG — Service is included in the composite surgical/procedural fee.
- QH — Independent procedures are not payable with other services.
- QI — 13612 is per laceration. If resubmitting, bill each laceration separately, and state length of any over 5 cm.
- QJ — Adjusted to agree with the surgical/assist fee item paid for this date of service.
- QK — Assistance at surgery/diagnostic procedures usually performed by one physician is not payable.
- QL — Assists and visits are not paid together unless distinct unrelated times are provided.
- QM — Multiple procedures at the same time, the lesser fee(s) paid at 50%.
- QN — Fee item requires pre-authorization. Please resubmit with the operative/procedural report and provide details regarding the medical necessity.
- QO — A claim for surgical fee item G04705, G04707 or G04709 has not been received. Therefore, this gynaecological certified assist fee item is not applicable.
- QP — Repeat/staged procedures are not paid within designated time limit.
- QQ — 77043 is not applicable according to the information provided.
- QR — A surgical surcharge is not applicable as the procedure billed is not considered a surgical item.
- QS — 07019/70019/70020 requires confirmation of medical necessity from surgeon.
- QT — Payment at 75% is not applicable.
- QU — Unassociated multiple procedures at the same time, the lesser fee is paid at 75%.
- QV — A claim for surgical fee item G04709 has not been received, therefore G04713 second surgical assist is not applicable.
- QW — Pre-approval is required for this fee item. Please resubmit upon approval.
- QX — A new authorization is required after two years per Preamble D.9.1.1. Please re-bill after a new authorization is received, if applicable.
- QY — ICBC refusal. No refusal reason code.
- QZ — 77043 is only paid with applicable vascular surgery items.
- Q1 — Long-term care institution visits have been paid during the time you are billing for home visits. Please verify location of service.
- Q2 — Home visits have been paid during the time you are billing for long-term care institution visits. Please verify location of service.
- Q3 — Fee item 13338 has been refused or debited as the corresponding hospital visit has been refused or debited.
R
- RA — Claim has been paid under the composite fee 08547 which includes 08530, 08537, 08544 and 08545.
- RB — X-rays billed by non-certified radiologists are paid at 75%.
- RC — Your re-billing has been refused. A retroactive adjustment will be made on a future remittance statement.
- RD — Payment has been reduced as this fee item is paid on a “per case basis”.
- RE — Encounter received.
- RF — Encounter required – patient registered to primary care organization.
- RG — Encounter record converted to fee for service.
- RH — Amount greater than $0 billed on an encounter record.
- RI — RGP fee for service. Claims are not valid for dates of service greater than June 30, 1995.
- RJ — Registration must be submitted by a medical doctor.
- RK — Fee for service record converted to an encounter record.
- RL — Payable only for approved procedures.
- RM — The miscellaneous fee item billed has been changed to this established fee item.
- RN — Dental/oral surgery with extractions – the higher gross fee item(s) are paid at 100% and extractions in the same quadrant paid as “each additional tooth”.
- RO — Multiple dental/oral surgeries are paid as the larger fee at 100%; the lesser fee at 50% unless otherwise stated in the MSP Dental Schedule.
- RQ — This fee item is payable once per jaw.
- RS — A claim for this service has been paid within the previous 12 months.
- RT — A claim for this service has been paid within the previous 12 months to another practitioner.
- RU — Amounts greater than $0 are not billable under this PHN.
- RW — This item is not applicable unless continuous time is spent with the patient.
- RX — Critical care fees are not applicable when the service starts after 2200 hours.
- RY — The maximum rate paid for these multiple laparoscopic operations is the rate payable for fee item 04229. This service exceeds the maximum.
- RZ — A visit is not payable in addition to an OSMV or MHR form fee when the patient is seen for the same diagnosis.
- R1 — (567) WorkSafeBC payment amount reduced to BC rates.
- R2 — (154) WorkSafeBC refused your claim submission. Transmitted record had a date of service prior to the date of birth.
- R3 — (536) WorkSafeBC penalty applied for service timeliness. Please refer to contract for more information.
- R4 — (569) WorkSafeBC claim cannot be matched at this time. Please contact payment services at 604 276-3085 or 1 800 422-2228.
S
- SB — WorkSafeBC refused your claim submission – concurrent treatment not authorized. If clarification required contact WSBC adjudicator.
- SD — (522) WorkSafeBC claim decision is pending. Please resubmit when claim status is accepted.
- SE — (523) WorkSafeBC service is not allowed with another service already entitled on this claim. Please refer to contract for contract terms.
- SF — (526) WorkSafeBC invoice date is greater than 90 days from date of service.
- SJ — (518) WorkSafeBC proof was not received or not accepted. Please check contract for proof requirements.
- SM — Your claim has been refused. Please resubmit with WorkSafeBC fee item for WorkSafeBC services.
- SN — This service is the responsibility of WorkSafeBC. Please resubmit with “WC” insurer code.
- SR — Invalid fee item for WorkSafeBC claim. Please resubmit using the appropriate MSP/WorkSafeBC fee item.
- SX — (551) WorkSafeBC payee not contracted to provide service.
- SZ — WorkSafeBC refused claim. Invalid body part code. Please resubmit with amended information.
- S1 — (146) WorkSafeBC refused claim. Invalid nature of injury code. Please resubmit with amended information.
- S2 — (148) WorkSafeBC refused claim. Invalid side of body code. Please resubmit with amended information.
- S3 — (542) WorkSafeBC payee could not be matched.
- S7 — (155) WorkSafeBC refused you claim submission. Transmitted record had a date of injury prior to the date of birth.
T
- TA — Patient’s annual limit for this benefit has been reached.
- TB — This fee is paid only once per patient, per year.
- TC — Balance owing on previously paid account.
- TD — Less than 3 months have elapsed since the last visit for this condition.
- TE — Less than 21 days have elapsed since the last visit for this condition.
- TF — Less than 3 months have elapsed since the last paid treatment.
- TG — As no authorization has been received, your account has been refused.
- TH — Fee item 02897 is included in fee items 02888, 02889, 02898 and 02899.
- TJ — Invalid phn/fee item combination: PHN XXXXXXXXXX only valid for fee 14010, PHN XXXXXXXXXX only valid for fee items 36062, 36063, 36064, 36065
- TK — This item is not applicable until the MSP age appropriate counselling fee item (00120, etc) calendar year limit (4) has been utilized.
- TL — ICBC approved claim with referring doctor number 99990.
- TM — ICBC approved claim with referring doctor number 99995.
- TO — This claim is the responsibility of ICBC.
- TP — Previous visit within 6 months for same condition.
- TR — ICBC claim is outside of approved treatment dates.
- TS — Payment has been made in accordance with the information provided by the referring physician.
- TT — Authorized payment amount has been reached.
- TU — Details required for frequency of servicing. Please resubmit with explanation in note record.
- TV — Service included in initial examination.
- TW — Payment has recently been made to other optometrist for this service.
- TX — ICD9 code does not match published list.
- TZ — Retroactive adjustment.
- T0 — Fee item 02888, 02889, 02898 and 02899 are included in fee items 02894 and 02895.
- T1 — Extractions in conjunction with osteotomies/fractures – bill extractions as “each additional tooth per quadrant” regardless of the number of quadrants involved.
- T2 — Please resubmit with location of extraction, lesion, etc.
- T3 — A1234565 is not an acceptable ICBC claim number
- T4 — ICBC refused. This may be a WorkSafeBC claim.
- T5 — Services exceed ICBC coverage limit.
- T6 — ICBC refused responsibility. Please contact adjuster
- T7 — Therapy treatment discontinued by medical practitioner. Please contact ICBC.
- T8 — Claimant has private plan for therapy. Please contact ICBC.
- T9 — ICBC customer unknown – please contact ICBC.
U
- UA — This claim was assessed by the Plan’s Medical and Surgical Advisors.
- UB — Claim has been paid/refused pending review by our Medical Advisors. You will be notified of any changes.
- UC — If you disagree with the payment made, please refer to the appropriate committee of the Doctors of BC (BCMA).
- UD — Paid according to Reference Committee recommendations.
- UE — Computer processed in accordance with Medical Services Commission Payment Schedule.
- UF — Invalid MVA – no injury claim.
- UG — Breach of ICBC coverage.
- UH — MVA prior to April 1, 1994. Contact ICBC if necessary.
- UI — Duplicate KOL 35 – contact ICBC if necessary.
- UJ — No ICBC claim for PHN – use ICBC number. Contact ICBC if necessary.
- UL — (515) WorkSafeBC the maximum service units entitled have already been invoiced. Contact claim owner for more information.
- UM — (513) WorkSafeBC service is not entitled on claim.
- UP — Claim refused as ICBC responsibility. Please re-bill ICBC directly or if patient qualifies for MSP therapy benefits, please bill MSP. ICBC claim # not required.
- UQ — This claim has been paid on an independent consideration and without precedent basis after review by MSP’s Medical and Surgical Advisors.
- U1 — Patient benefit limit reached – refractions are only payable once every 24 months for patients between the ages of 16 and 64.
- U2 — A refraction has been previously paid to a different specialty – refractions are only payable once every 24 months for patients between the ages of 16 and 64.
- U3 — Insufficient information has been provided to authorize a repeat refraction within 24 months.
- U4 — Routine eye examinations are not a benefit of MSP.
- U5 — Insufficient medical necessity provided for a repeat eye examination for the diagnosis indicated.
V
- VA — Payment number is missing or invalid.
- VC — Payment number not valid for this batch.
- VE — Amount billed is missing or invalid.
- VF — Number of services is missing or invalid.
- VG — Fee item is missing or invalid.
- VH — Date of service is missing or invalid.
- VI — Practitioner number is missing or invalid.
- VJ — Invalid diagnostic code for referral by oral/dental surgeon or orthodontist. Diagnosis must relate to problems with mouth or mastication.
- VK — Claim number is missing or invalid.
- VL — Claim number is out of sequence.
- VM — Referring practitioner number is missing or invalid.
- VN — Diagnostic code missing or invalid.
- VO — Anatomical position invalid or missing.
- VP — Service to-date missing or invalid.
- VQ — The number of services exceeds the maximum allowed.
- VR — Critical care must be submitted on a claim card with a covering letter providing the details.
- VS — The to/by indicator for the referring doctor is invalid.
- VT — Claim has been paid/refused pending review. You will be notified of any changes.
- VU — Nature of injury missing or invalid.
- VV — Date of injury missing or invalid.
- VW — WorkSafeBC claim number missing or invalid.
- VX — Medical practitioner referral required by ICBC. Please contact ICBC.
- VY — Area of injury missing or invalid.
- VZ — ICBC claim number invalid for WORKSAFEBC claim.
- V0 — Invalid diagnostic code for referral to an otolaryngologist from a dentist or paediatric dentist. Diagnosis must relate to neoplasms of lip, oral cavity or pharynx.
- V2 — Reserved for ICBC misc. adjustments where two bills are sent for one service.
- V3 — Field(s) designated for future use contain(s) invalid data – refer to current Teleplan specs.
- V4 — (553) WorkSafeBC invoiced amount paid.
- V7 — Services referred by de-enrolled practitioners are not a benefit of MSP.
- V8 — Paid according to your MSP orthodontia contract.
- V9 — This patient is not user fee exempt for this date of service.
W
- W$ — Work Safe BC claim submitted to Work Safe BC on paper.
- WA — Service not approved for this payment number or date of service prior to approval date
- WB — (541) WorkSafeBC claim could not be matched.
- WC — Fee item not listed with Medical Services Plan.
- WD — (511) WorkSafeBC claim rejected or disallowed. Do not rebill.
- WE — Hospital payee claim submission refused. Bill WorkSafeBC directly.
- WF — Fee item billed and doctor’s specialty/practitioner number do not correspond.
- WG — Fee items with letter prefix ‘A’ are not benefits of the Plan.
- WH — We are unable to process a single claim for two different patients.
- WI — Billing is incomplete. Please resubmit with all required information.
- WK — Please re-bill with initial fee for the first service and the additional fee for each additional service performed.
- WN — Pre-authorization number valid.
- WO — Pre-authorization number invalid.
- WP — Pre-authorization permits payment of this inactive coverage.
- WQ — WorkSafeBC refused your claim submission – approval outstanding, pending time exceeded. Please resubmit using code “W”.
- WR — Pre-authorized number invalid.
- WS — (561) WorkSafeBC service prior to injury.
- WT — Tray fee not applicable to procedure billed. Refer to the list of procedures eligible for a tray fee in the General Services Section of MSC Payment Schedule.
- WU — Unknown reason for refusal or change to fee item and/or amount. Please contact WorkSafeBC.
- W0 — Work Safe BC refused your claim submission – report incomplete. If clarification required contact WorkSafeBC Payment Services.
- W1 — Postal code missing or format invalid.
- W2 — Data centre and payee number combination not on file.
- W3 — Payee not active.
- W4 — Use claims comment or note record. Please do not use both.
- W5 — Note data type not equal to “A”.
- W6 — Note data line blank (no data).
- W7 — Provincial institution not applicable for batch eligibility.
- W8 — Dependent 66 not applicable for batch eligibility.
- W9 — Greater than three errors for this claim.
X
- XA — RCP claims – birthdate and sex code missing or invalid.
- XB — Eligibility Request – invalid patient status request code used.
- XC — Eligibility Request – invalid sex code.
- XD — Invalid/insufficient information provided. (In note or claim comment field/description area.)
- XE — Practitioner does not have approval for this service.
- XF — Facility does not have approval for this service.
- XG — Note comment does not correspond with submission code.
- XH — This claim has been returned to you per your submission code E request record.
- XJ — Please resubmit on the appropriate claim card/online form.
- XK — RCP/Registration Number is not numeric or is equal to zero.
- XL — WorkSafeBC claim number has been added/updated. Please contact WorkSafeBC for correct claim number.
- XM — PCO – ICBC has refused responsibility for this claim.
- XN — PCO – encounter record created to replace fee for service claim refused by ICBC.
- XP — ICBC refused – claim processed by MSP.
- XW — Expedited WorkSafeBC surgical premium applied.
- XY — Vendor test record returned.
- X0 — Facility – Prac or Payee not connected
- X1 — Original MSP file number invalid.
- X2 — Facility number is missing or invalid.
- X3 — Sub-facility number is missing or invalid.
- X4 — RCP/Institution number missing, invalid, or not in correct format.
- X5 — RCP/Institution birthdate missing or invalid.
- X6 — RCP/Institution first name missing or invalid.
- X7 — RCP/Institution second initial invalid.
- X8 — RCP/Institution – patient sex code missing or invalid.
- X9 — RCP address missing or not showing in line one.
- X# — Invalid sub-facility for this service type.
Y
- YA — Note record missing or invalid for submission code C, E or X.
- YB — This Teleplan record code is not operational. Please contact Teleplan Support.
- YC — Claim number refused by ICBC. Please contact ICBC.
- YD — Insurer code does not match fee item billed. This fee item is only applicable for ICBC billings.
- YF — Fee item valid for WorkSafeBC claim only
- YH — No payment owing. Insurer code adjusted.
- YI — Provincial institution not valid for WorkSafeBC claim.
- YK — Claim reprocessed at the request of WorkSafeBC.
- YN — Newborns invalid for WorkSafeBC claim – DEP 66.
- YP — WorkSafeBC claim must be submitted by PHN.
- YR — Claim reprocessed/adjusted at the request of ICBC to change insurer responsibility.
- YS — Specialty invalid for WorkSafeBC claim.
- YT — WorkSafeBC claim must be Teleplan for opted in practitioner.
- YU — ICBC refusal reason unknown – Please contact ICBC.
- YV — Data Centre change. Record submitted by previous data centre being returned to new data centre.
- YW — Insurer responsibility switched at the request of ICBC.
- YX — Claim reprocessed at the request of ICBC.
- YY — Pre-Edit System refusal. See second explanatory code(s).
- YZ — Facilities edit refusal.
- Y1 — Billed fee prefix invalid.
- Y2 — Payment mode is invalid.
- Y3 — Submission code invalid.
- Y4 — Service location code missing or invalid.
- Y5 — Referring practitioner code 1 missing or invalid.
- Y6 — Referring practitioner code 2 missing or invalid.
- Y7 — Correspondence code invalid.
- Y8 — MVA claim code invalid.
- Y9 — ICBC claim number invalid.
Z
- ZI — Note record is not preceded by correspondence code equal to “N” or “B” or practitioner number does not match C01/C02 record.
- ZJ — PHN equals zero and province code equals zero or blanks.
- ZK — A note record did not accompany correspondence code “N” or “B” or payee number does not match C02 record.
- ZL — RCP province code is present and PHN not equal to zero.
- ZM — Coverage good – batch eligibility. This code is used in Teleplan II.
- ZN — No coverage – batch eligibility. This code is used in Teleplan II.
- ZS — The referring doctor number has been changed to correspond with our records.
- Z5 — Referring doctor number has been changed to correspond with our records.
- Z8 — Unable to process Ir1 or Ir2 record, zero payments returned to ICBC.
- Z9 — ICBC reversal request denied – MSP staff or data centre adjustment already created.
0-9
- 0B — Provincial coverage limits payment to $75 CDN for out of country MRI scans.
- 1B — This fee item not valid for services provided in BC. Please resubmit with appropriate fee item.
- 1W — WorkSafeBC claim submitted to WorkSafeBC on paper – Work Safe BC adjusted – keying fee deducted.
- 2A — Chiropractic, Naturopathic, Optometric, Physiotherapy, Massage Therapy, Podiatry and Acupuncture services are not insured benefits outside of BC.
- 2W — WorkSafeBC Claim – Invalid PHN
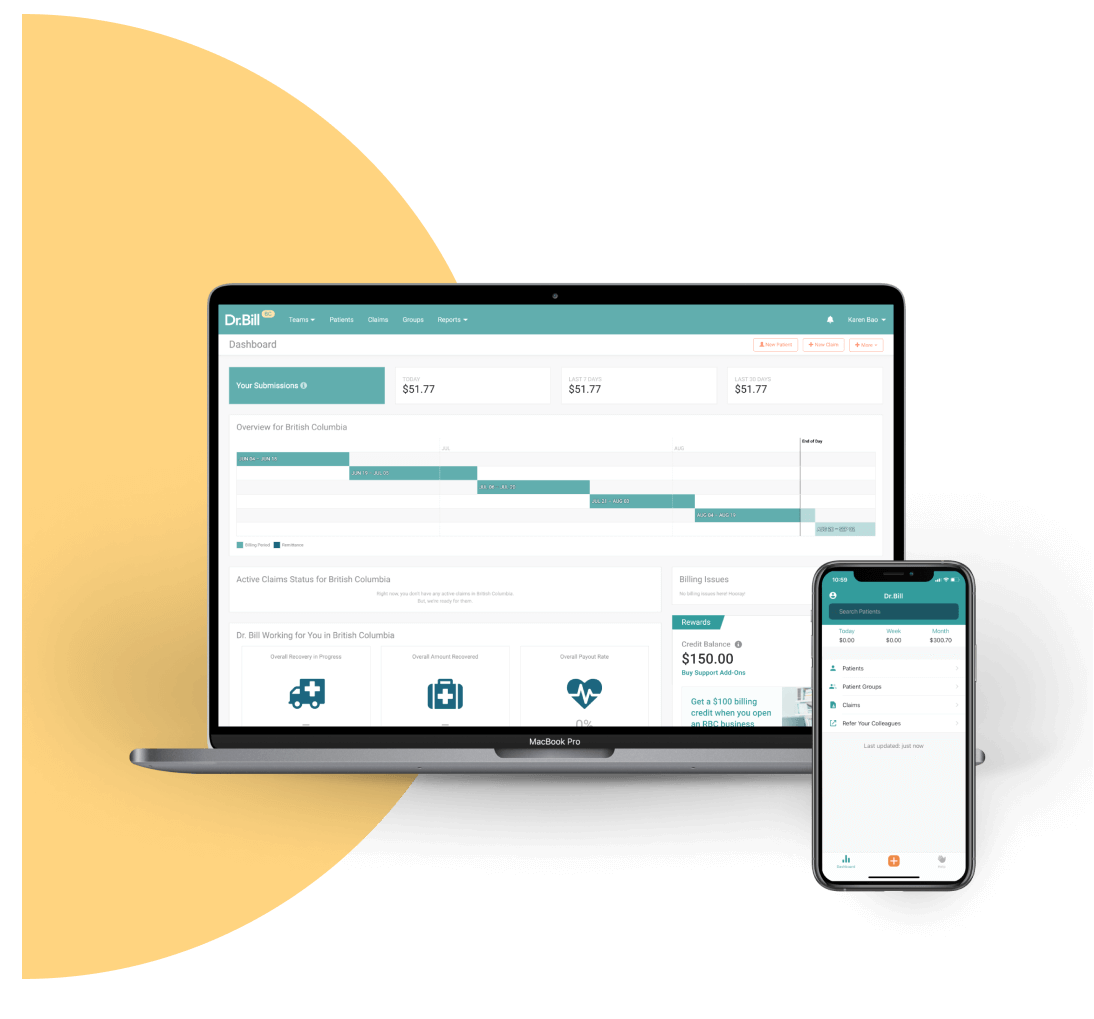
An MSP Expert in your Pocket
Find codes and bill premiums with a tap. Get a $150 Credit when you sign up for Dr.Bill*.





